Nursing Informatics Series: Lynn’s Journey

Today, as a Senior Nurse Informaticist at Lantana, I am part of a team of clinical, program and policy analysts, working with IT engineers to develop standards-based solutions permitting interoperable—platform independent—exchange of health information. Twenty-five years ago, I was a young nurse starting out—just look at me here at my “capping and pinning” ceremony! Here is the story of my nursing journey into informatics.
Back then, I thought nursing was all about providing great hands-on patient care. Little did I know of the documentation burden that came heavy with the job—because in nursing, “if it isn’t documented, it didn’t happen.” I vividly recall the many hours spent on paperwork after my shift ended: sorting through piles of handwritten notes on scraps of paper, deciphering the smeared ink notes on my arms, and waiting for others to finish with the paper chart so I could have my turn.
By the late 1980’s, computers became part of the health care landscape, but their potential for easing the documentation burden never seemed to materialize. Computerized order entry—for things like nutrition, labs, and x-rays—became widely adopted, but recording the patient encounter remained stuck in the world of paper, clipboards and file cabinets. When I moved from a hospital to a multi-specialty clinic, my frustration with documentation was worse than ever. In the outpatient setting, charts commonly were missing notes from previous visits, or just missing entirely—moved to other locations or not forwarded—filed somewhere other than where they were really needed. The process seemed needlessly burdensome and inefficient. I wanted to be focused on providing quality patient care, not chasing down missing records and having to make questionable clinical choices because of inadequate information. What to do? Grumble and complain? I wanted to do something – after all, “If you’re not part of the solution, you’re part of the problem,”—but what? I began looking for opportunities to play a role in fixing the documentation tangle, and soon was working with the clinic’s quality improvement committee and pushing for online clinical documentation within our electronic medical record.
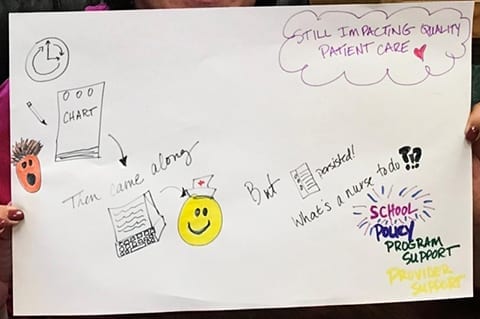
My journey– from hands-on care and handwritten charting to embracing technology
for health information management that improves patient care quality.
Several years later, I found myself “on the other side” of health care, still engaged in quality improvement, but this time helping hospitals and clinicians implement quality reporting and patient safety programs. My work on a quality measure reporting tool impressed on me the direct relationship between clinical care, the data that was generated, and how that data informed decisions about care quality. This interest spurred me on to complete a graduate degree in nursing informatics.
I provide clinical subject-matter expertise on hospital and clinician quality reporting, develop and maintain electronic clinical quality measures, and support federal reporting program rulemaking. It’s satisfying to be directly involved in the transformation of health care, to be doing work that aligns with my desire to improve quality patient care using efficient and effective information management.
I know some will say the documentation burden has not decreased at all, but that it’s simply changed form. There is no question that much remains to be done. But look at how far we’ve come! To have immediate access to the medical record, to document in real-time, and to be able to read and share patient documentation—all of this is should be welcomed as a positive change in the health care workflow and in facilitating the delivery of high-quality clinical care.